RELATED STORY:
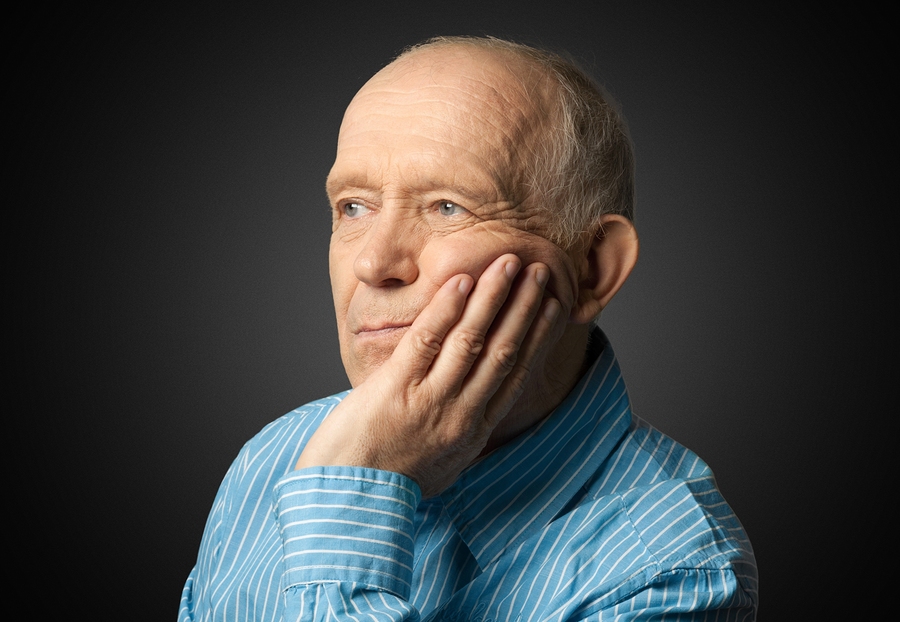
As I discuss in my video Cholesterol & Alzheimer’s Disease “[c]onsiderable evidence now indicates that Alzheimer’s disease (AD) is primarily a vascular disorder,” based on a number of lines of evidence that point toward impaired circulation of blood to the brain. Vascular risk factors, such as high cholesterol, can be thought of as a ticking time bomb to Alzheimer’s disease. What’s bad for the heart may be bad for the mind.
Traditionally, there have been two competing theories for the cause of Alzheimer’s: the amyloid cascade model, which implicates the buildup of amyloid plaques within the brain, and the vascular model, which argues that it is the lack of adequate blood flow to the brain due to atherosclerosis. We now realize they are not mutually exclusive and that arterial disease can set up a vicious cycle in which atherosclerotic plaques in the arteries may contribute to Alzheimer’s plaques in the brain.
Although cholesterol has been portrayed as “tantamount to poison,” it is an essential structural component of all of our cells, and that’s why our body makes it. But, if there’s too much, it can become a major factor contributing to various diseases, including coronary heart disease, stroke, and neurodegenerative diseases like Alzheimer’s. Too much cholesterol in our blood is universally recognized to be a risk factor for the development Alzheimer’s disease, and cholesterol may play an active role in the progression of Alzheimer’s as well.
Autopsy studies have found that Alzheimer’s brains have significantly more cholesterol than normal brains, and it specifically appears to accumulate in the Alzheimer brain plaques. We used to think the pool of cholesterol in the brain was separate from the pool we had in our blood, but there is now growing evidence to the contrary. For example, low-density (LDL) cholesterol, the so-called bad cholesterol, may be able to cross the blood–brain barrier into the brain. So, a high-fat diet may not only increase cholesterol levels in the blood, but also the influx of cholesterol into the central nervous system.
In addition, having high cholesterol may even damage the blood-brain barrier itself, and allow for even more cholesterol to flow into the brain, providing the missing link between high cholesterol and Alzheimer’s. “Individuals with higher cholesterol levels at midlife have a higher risk of developing [Alzheimer’s disease].” Cholesterol over 250 could potentially triple the odds of Alzheimer’s.
We now have high-tech PET scanning of the brain that can directly correlate the amount of bad LDL cholesterol in our blood with the amount of amyloid buildup in our brains. You can even do it right in a petri dish. Adding cholesterol makes brain cells churn out more of the amyloid that makes up Alzheimer plaques, whereas removing cholesterol can decrease the levels of amyloid released from cells.
Amyloid degradation is also less efficient in a high cholesterol environment. Cholesterol can then help seed the clumping of the amyloid. Using an electron microscope, researchers can see the clustering of amyloid fibers on and around little microcrystals of cholesterol.
Once in the brain, cholesterol can also undergo auto-oxidation, causing the formation of highly toxic free radicals. So, having high cholesterol levels in the blood is thought to increase the risk of dementia, not only by inducing atherosclerosis and impairing blood flow, but also by potentially directly affecting neurodegeneration within the brain. In conclusion, excess dietary cholesterol could, in principle, contribute to the development of Alzheimer’s disease, and the evidence linking high cholesterol to Alzheimer’s appears to be steadily mounting.
Some of this work was paid for by drug companies hoping to capitalize on Alzheimer’s with cholesterol-lowering statin drugs. This is ironic, since statins themselves can cause cognitive impairment. Though rare, statin side effects may “include short- and long-term memory loss, behavioral changes, impaired concentration and attention, paranoia, and anxiety,” as early as five days after starting the drugs, but sometimes even months later, though folks should recover within a month of stopping the drugs.
RELATED STORY:
A better strategy may be to change the lifestyle factors that lead to the high cholesterol in the first place—in particular, reducing saturated fat in the diet. It’s not enough for us to just tell our individual patients, though. “Systematic implementation of educational campaigns promoting radical changes in cultural and societal values” may be necessary to adopt Alzheimer’s-defeating strategies by patients in a broader sense, and “such actions may provide potentially huge dividends by preventing both cardiovascular disease and dementia”—two of our leading causes of death.
In health,Michael Greger, M.D.
*Article originally appeared at Nutrition Facts.