In 1901, Auguste was taken to an insane asylum in Frankfurt, Germany, by her husband. She was described as a delusional, forgetful, disoriented woman who “could not carry out her homemaking duties.” She was seen by a Dr. Alzheimer and was to become the case that made his a household name.
On autopsy, he described the plaques and tangles in her brain that would go on to characterize the disease, but in the excitement of discovering a new entity, a clue may have been overlooked. He described arteriosclerotic changes—hardening of the arteries—within her brain.
RELATED STORY:
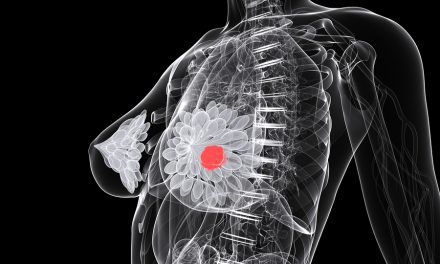
We typically think of atherosclerosis in the heart, but atherosclerosis involves virtually the entire human organism—our entire vascular tree. One of the most poignant examples of this systemic nature is the link between coronary artery disease, degenerative brain disease, and dementia.
Back in the 1970s, the concept of “cardiogenic dementia” was proposed—dementia generated from the cardiovascular system. Since the aging brain is highly sensitive to lack of oxygen and since heart problems are so common, it was easy to imagine that’s how dementia could result. Now we have a substantial body of evidence that strongly associates atherosclerotic vascular disease with the number one cause of dementia, Alzheimer’s disease. Autopsy studies, for example, have shown that individuals with Alzheimer’s have significantly more atherosclerotic narrowing of the arteries within their brain.
In my Alzheimer’s and Atherosclerosis of the Brain video, you can see what cerebral arteries should look like—open and clean, allowing blood to flow—versus what atherosclerosis in our brain arteries looks like—clogged with fat and cholesterol, closing off the arteries, and restricting blood flow to our brain. It’s really a remarkable compelling comparison—I encourage you to check it out.
RELATED STORY:
What kind of brain arteries do you want in your head?
The normal amount of blood circulating within our brains is about a quart a minute, but we lose about a half-percent a year; by age 65 we may be down 15-20%. This doesn’t necessarily affect brain function since we have a built-in buffer. However, this age-related decline in cerebral blood flow can become critical to brain cell survival if an additional burden further lowers flow. This reduction of blood flow can starve the brain of oxygen, cause silent little mini-strokes and brain atrophy, the cumulative effects of which appear to play a pivotal role in accelerating and augmenting the development and evolution of Alzheimer’s disease.
As shown in Alzheimer’s and Atherosclerosis of the Brain, you can see the vast difference in the amount of atherosclerosis in the arteries that specifically supply blood to critical memory and learning centers of the brain of healthy, non-demented controls compared to those with Alzheimer’s disease. In light of such findings, some have even suggested the disease be reclassified as vascular disorder.
This is good news, though, because atherosclerosis is potentially reversible. These findings were confirmed in two larger studies of more than 1,000 autopsies each, which found the same thing. Atherosclerosis in the brain is significantly more frequent and severe in those with Alzheimer’s disease.
This suggests that strategies proven to delay the progression of artery disease like plant-based diets may be useful for preventing or treating Alzheimer’s disease. Of course, autopsy studies are a little late for that, so to assess the impact of intracranial arterial narrowing on the progression from mild cognitive impairment to Alzheimer’s disease, researchers followed 400 people with cognitive impairment for four years using CT angiography—special CAT scans that evaluate the amount of brain artery blockage. The cognition of those with the least atherosclerosis in their heads remained pretty stable over the years, but those with more cholesterol buildup got worse and those with the most blockage rapidly declined. The ability to carry on the activities of daily living was also affected, and the progression to Alzheimer’s disease was doubled. An inefficient blood supply to the brain has very grave consequences on brain function.
RELATED STORY:
But does treatment of vascular risk factors like high blood pressure and high cholesterol actually make a difference? We didn’t know, until a recent study of 300 patients with Alzheimer’s. Those with all their vascular risk factors treated showed significantly less decline and slowed progression of their disease, compared with those who went untreated.
It’s been said that the “goal of medicine is to provide patients with hope and when there is no hope, to offer understanding.” Well, for the first time in the history of this disorder, we have the chance to provide Alzheimer’s patients with hope.