(Editor’s Note: Erin’s editor here- I have had verifiable endometriosis for almost 4 years now and my latest scans show that the endo that was in my right ovary is totally gone and the endo in my left ovary has shrunk by over half. Just over two years ago I dramatically changed my diet by becoming a vegan. I also exercise 3 to 5 days a week and have gotten rid of all chemical cleaning and personal products, as well. I lost weight, feel amazing, and do not suffer the symptoms of my disappeared endo. Please know, there is hope.)
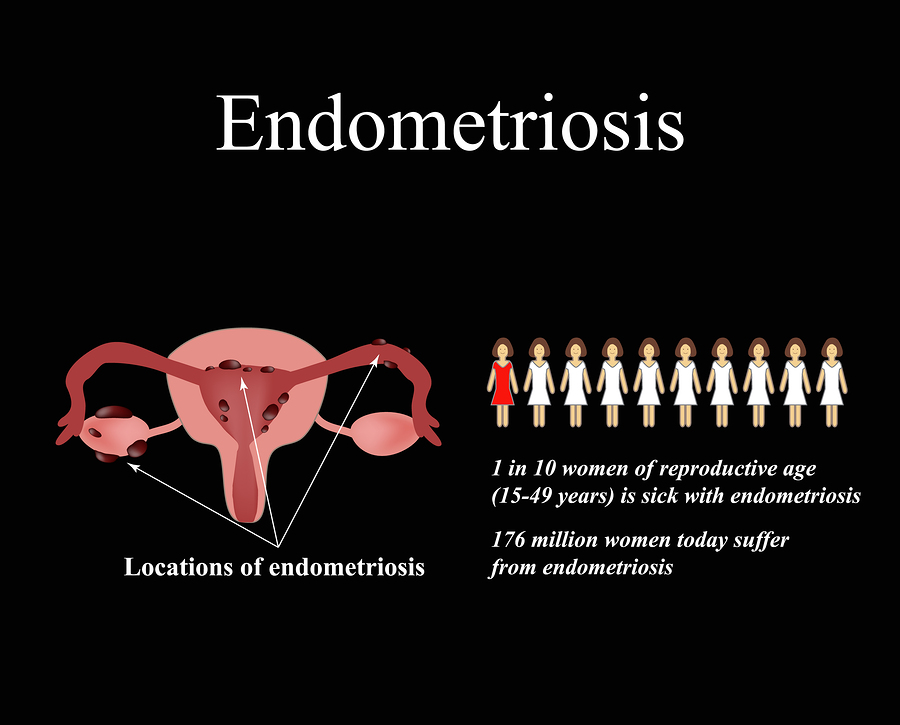
Endometriosis is estimated to affect as many as one in 10 women worldwide.
It’s a disease involving the reproductive system in which endometrium-like tissue grows outside the uterus in areas like the ovaries, abdomen, and bowel. Normally, endometrial tissue is only found inside the uterus.
Symptoms include painful periods and heavy bleeding, pain during intercourse, painful bowel movements and infertility.
The cause of endometriosis is unknown, and there is currently no cure.
However, certain foods may increase or decrease the risk of endometriosis, and some women find that making dietary changes can help reduce symptoms.
Here are 8 diet changes that may aid in managing endometriosis.
1. Increase Your Intake of Omega-3 Fats
Omega-3 fats are healthy, anti-inflammatory fats that can be found in fatty fish and other animal and plant sources.
Certain types of fats, such as plant oils containing omega-6 fats, may promote pain and inflammation. However, omega-3 fats are believed to have the opposite effect, acting as the building blocks of your body’s inflammation- and pain-relieving molecules.
Given that endometriosis is often associated with increased pain and inflammation, having a high ratio of omega-3 to omega-6 fats in the diet may be especially beneficial for women with this disease.
What’s more, a high ratio of omega-3 to omega-6 fats has been shown to inhibit the survival of endometrial cells in test-tube studies. Preliminary evidence suggests that omega-3 fats might help discourage the implantation of endometrial cells in the first place.
Furthermore, one observational study found that women who consumed the highest amounts of omega-3 fats were 22% less likely to have endometriosis, compared to women who consumed the lowest amounts.
Lastly, researchers have found that taking fish oil supplements containing omega-3 fats may significantly decrease menstrual symptoms and pain.
However, the evidence is inconclusive. Other observational studies have found no association between fat intake and the risk of endometriosis.
Nevertheless, whether you eat more fatty fish or take omega-3 supplements, increasing your intake of these fats is one of the simplest dietary changes you can make to fight endometriosis-associated pain and inflammation.
SUMMARY:Omega-3 fats have anti-inflammatory properties, and they have been shown to help decrease period pain. What’s more, a high omega-3 fat intake has been associated with a reduced risk of endometriosis.
2. Avoid Trans Fats
In recent years, trans fats have become infamous for being unhealthy.
Research has found that trans fats increase levels of “bad” LDL cholesterol and decrease “good” HDL cholesterol, thus increasing the risk of heart disease and death.
Trans fats are created when liquid unsaturated fats are blasted with hydrogen until they become solid. Manufacturers typically create trans fats to give their products a longer shelf life and more spreadable texture.
This makes them perfect for use in a variety of fried and processed items, such as crackers, donuts, fries, and pastries.
However, beginning in 2018 the US Food and Drug Administration (FDA) will ban trans fats in all food products due to the danger they pose to health. Until then, it’s prudent to avoid products containing trans fats.
In particular, women with endometriosis should avoid them. One observational study found that women who ate the highest amounts of trans fats had a 48% increased risk of endometriosis.
One study is by no means conclusive, but avoiding trans fats is a good recommendation regardless.
You can tell if a product has trans fats by reading the label. Anything containing partially hydrogenated fats contains trans fats too.
SUMMARY:Trans fats, which are found in some processed foods, increase the risk of heart disease. Some evidence has also shown that they may increase the risk of endometriosis.
3. Cut Down on Red Meat
Red meat, especially processed red meat, has been linked to a higher risk of certain diseases. In fact, replacing red meat with another protein source may improve inflammation, which is often associated with endometriosis.
Additionally, one observational study found that women who ate more meat and ham had an increased risk of endometriosis, compared to those who ate little meat or ham.
RELATED STORY
However, two other studies failed to find the same result.
Some evidence suggests that a high intake of red meat may be associated with higher levels of estrogen in the blood.
Since endometriosis is an estrogen-dependent disease, higher levels of estrogen in the blood may increase the risk of the condition.
There is currently not enough research about red meat and endometriosis to make a solid recommendation.
Even though current evidence is conflicting, some women may benefit from reducing their red meat intake.
SUMMARY: Red meat has been associated with a higher risk of endometriosis in some studies. It may also lead to increased estrogen levels.
4. Eat Plenty of Fruits, Vegetables, and Whole Grains
Fruits, veggies and whole grains are packed with vitamins, minerals, and fiber.
Filling your plate with a combination of these foods ensures that your diet is packed with essential nutrients and minimizes your intake of empty calories.
These foods and their benefits may be especially important for those with endometriosis.
Dietary fiber is believed to help the body excrete hormones from the body, and studies have associated a high fiber intake with lower blood levels of sex hormones, including estrogen.
This means eating a high-fiber diet may be an excellent strategy for women with endometriosis.
RELATED STORY:
Fruits, vegetables, and whole grains are the best sources of dietary fiber. These foods also provide antioxidants, which may also help combat inflammation.
One study found that women with endometriosis who followed a high-antioxidant diet for four months experienced increased antioxidant capacity and decreased markers of oxidative stress.
Another study found that taking antioxidant supplements significantly decreased endometriosis-related pain.
One study directly investigated the relationship between endometriosis and eating fruits and green vegetables. It found that a higher intake of these foods was associated with a lower risk of the condition.
However, findings have not been consistent. Another study found that high fruit intake was associated with an increased risk of endometriosis.
One possible explanation is that eating more fruit often comes with increased pesticide consumption. Certain types of pesticides may have estrogen-like effects, which could, in turn, affect endometriosis.
Without more research, it’s not possible to say for sure how fruit and vegetable intakes affect endometriosis. Yet, current evidence suggests that following a diet rich in fruits, vegetables, and whole grains may be a good strategy.
SUMMARY:Fruits, vegetables and whole grains are packed with dietary fiber, which may help decrease estrogen concentration in the body. They also provide vitamins, minerals and antioxidants, which may help fight pain and oxidative stress.
5. Limit Caffeine and Alcohol
Health professionals often recommend that women with endometriosis reduce their caffeine and alcohol intakes.
Several studies have found that women with endometriosis tend to consume higher amounts of alcohol than women without the disease.
Yet, this doesn’t prove that high alcohol intake causes endometriosis. For example, it could mean that women with endometriosis tend to drink more alcohol as a result of the disease.
Furthermore, several other studies have found no link between alcohol intake and endometriosis.
Similarly, the potential link with caffeine is unclear.
While a few studies have found that caffeine or coffee intake was associated with a higher risk of endometriosis, a large review found that caffeine intake does not increase the risk of the condition.
Despite these results, alcohol and caffeine intake have both been associated with increased levels of estrogen, the protein that transports estrogen throughout the body.
RELATED STORY:
Although there is no clear evidence linking caffeine or alcohol to the risk or severity of endometriosis, some women still prefer to reduce or remove these substances from their diets.
SUMMARY:Some research suggests that caffeine and alcohol may increase the risk of endometriosis. Also, a high caffeine intake may increase estrogen levels. While this evidence is by no means conclusive, some women still prefer to reduce their intakes.
6. Cut down on Processed Foods
Minimizing your intake of processed foods is a good idea for almost anyone, and doing so may also help with the management of endometriosis.
Processed foods are often high in unhealthy fats and sugar, low in essential nutrients and fiber and may promote pain and inflammation.
RELATED STORY:
Omega-6 fats found in plant oils, such as corn, cottonseed, and peanut oil, can increase pain, uterine cramping, and inflammation.
On the other hand, omega-3 fats found in fish, walnuts, and flax may help reduce pain, cramping and inflammation.
As a result, limiting your intake of foods such as pastries, chips, crackers, candy and fried foods may help minimize endometriosis-related pain.
For even more impact, replace processed foods with those likely to help manage endometriosis, such as fatty fish, whole grains or fresh fruits and vegetables.
SUMMARY:Processed foods are low in important nutrients and fiber, and they often contain unhealthy fats and added sugars, both of which promote inflammation and pain.
7. Try a Gluten-Free or Low-FODMAP Diet
Certain diets may help reduce the symptoms of endometriosis.
Gluten-Free Diet
A gluten-free diet is not often recommended for individuals who do not have celiac disease or a specific gluten sensitivity. It is restrictive and can be low in fiber and nutrients, while high in refined starches.
However, there is some evidence that a gluten-free diet may benefit individuals with endometriosis.
One study in 207 women with severe endometriosis pain found that 75% of them experienced significant decreases in pain after 12 months on a gluten-free diet.
This study did not include a control group, so the placebo effect cannot be accounted for.
Nevertheless, another study in 300 women found similar results, and it did include a control group. One group took medication only, while the other group took medication and followed a gluten-free diet.
At the end of the study, the group following the gluten-free diet experienced significant reductions in pelvic pain.
Low-FODMAP Diet
The low-FODMAP diet may also be beneficial for women who have endometriosis.
This diet was designed to relieve intestinal symptoms in patients with irritable bowel syndrome (IBS). It requires avoiding foods high in FODMAPs, a term that stands for fermentable oligo-, di- and monosaccharides and polyols.
Gut bacteria ferment FODMAPs, resulting in the production of gas that causes pain and discomfort in those with IBS.
A study in people with either IBS or IBS and endometriosis found that a low-FODMAP diet improved IBS symptoms in 72% of those who had both endometriosis and IBS, compared to 49% in those with IBS alone.
Both the gluten-free diet and low-FODMAP diet can be restrictive and somewhat difficult to manage. However, they may offer relief for endometriosis symptoms.
If you decide to give one of these diets a try, it’s a good idea to meet with a dietitian to create a plan that works for you.
SUMMARY:A few studies have shown that a gluten-free diet may help reduce endometriosis symptoms, while a low-FODMAP diet may reduce IBS symptoms in women who have endometriosis and IBS.
8. Soy May Be Beneficial
Some endometriosis diets recommend eliminating soy from your diet. This is because soy contains phytoestrogens, which are plant compounds that can mimic estrogen.
However, it’s largely unknown how phytoestrogens affect endometriosis.
Some evidence suggests they may be harmful. One study found that women fed soy formula as infants had more than double the risk of endometriosis than women who were not fed soy formula as infants.
In addition, a few animal studies and case reports of women with endometriosis have reported negative effects associated with taking soy supplements.
Yet, many studies that have examined dietary soy intake in women with endometriosis have found exactly the opposite.
One study found that soy intake was not associated with the risk of endometriosis, and three other studies found that soy intake decreased the risk or severity of it.
Interestingly, a phytoestrogen called puerarin is currently being investigated in animal studies as a potential treatment for endometriosis.
Researchers have proposed that rather than increasing estrogen-like effects in the body, phytoestrogens have the opposite effect, blocking the effects of estrogen and contributing to endometriosis.
In general, estrogen binds to cell receptors that make up your tissues.
The effects of phytoestrogens are weaker than those of estrogen itself. So the reasoning goes that when phytoestrogens bind to estrogen receptors, fewer unoccupied receptors are available for estrogen to act on. This may result in an anti-estrogen effect in the body.
The little evidence that exists seems to support this theory. However, more research is needed before conclusions can be made about the effects of soy and other phytoestrogens on endometriosis.
SUMMARY:Some sources recommend avoiding soy, but it’s not clear whether this is a good recommendation. While some evidence suggests that soy may have negative effects on endometriosis, other studies have found that it decreases the risk of endometriosis.
The Bottom Line
There is no cure for endometriosis, and surgical or medical treatments remain the most effective methods of managing the condition.
However, making dietary changes is a complementary approach that may help some women manage their symptoms.
Keep in mind that just as symptoms of the disease vary from person to person, treatments that work best for one woman may not be right for another.
Take your time to experiment with the tips above to find the approach that’s right for you.